Papa is your strategic partner in the home. Our Papa Pals provide trusted, social support for Medicare Advantage, Medicaid, and Special Needs Health Plan members—filling gaps in support that lead to improved healthcare utilization, lower costs, and better health.

A configurable care network
We do what technology alone cannot—provide real human connection and support to address social determinants of health. Health plan clients can layer additional capabilities, such as post-discharge support, digital health literacy education, and in-home assessments, onto their core companion care program to drive even more value.
National footprint
Eyes and ears in the home
Last-mile support
Targeted enrollment
Add-on capabilities
Proven outcomes
Real impact powered by real people
Creating and scaling a category-defining model requires continual monitoring, measuring, and adapting based on results. With a long-time commitment to research and impact, Papa has a growing body of evidence—both in numbers and in smiles—that shows companion care’s clear value.
Reduced member churn3
-15.8%
Our technology
Tech has its place, even in companion care services. Our Papa Pals and Care Team are supported with our powerful social care platform—making it easy to connect, view visits, and provide feedback.
Intuitive app to empower our Papa Pals.
Our iPhone and Android apps provide Papa Pals easy access to everything they need to deliver a great experience to your members. They can see visit guidance, safety and educational content, health plan resources, and more. At the end of each visit they are able to report needs and risks back to use in a timely manner.
Online member portal.
Members can review, manage, and schedule upcoming Papa visits on the web at any time—no password required! Custom-built for older adults and individuals with varying levels of cognitive and physical abilities, Papa’s online member portal ensures all members can access our services in the way that’s best for them.
Tech-enabled social care platform.
Member needs identified by Papa Pals in the home, from our proprietary social needs assessments, or via eligibility file analysis are surfaced in real time for social care navigation or back to the health plan.
Detailed, timely reporting for clients.
We drive unique social health insights and outcomes, and we make sure it’s reported back to you. Regular dashboards are shared with clients and track program activity, identified gaps and referrals, member satisfaction, and more to track performance against goals.
How it works
Thousands of Papa Pals are working to lighten the load and brighten the day for members nationwide, in person or remotely. They offer companionship, provide encouragement, remove barriers, and help reduce the complexity of navigating technology and care.
Members sign up by phone with our Care Team.
Papa works with you to introduce the benefit and onboard eligible participants. We proactively reach out to members, increasing enrollment and utilization.
Members meet with Papa Pals.
Papa Pals browse visits on our platform and select the best fit based on preferences and availability. We keep track of the details, identify gaps, facilitate escalations, and provide companionship to improve engagement and adherence.
Member feedback and data drive ongoing improvements.
Post-visit, we gather member feedback on how their visit went. Papa Pals’ documentation of risks and needs helps us (and your health plan and insurance members) get better and better!

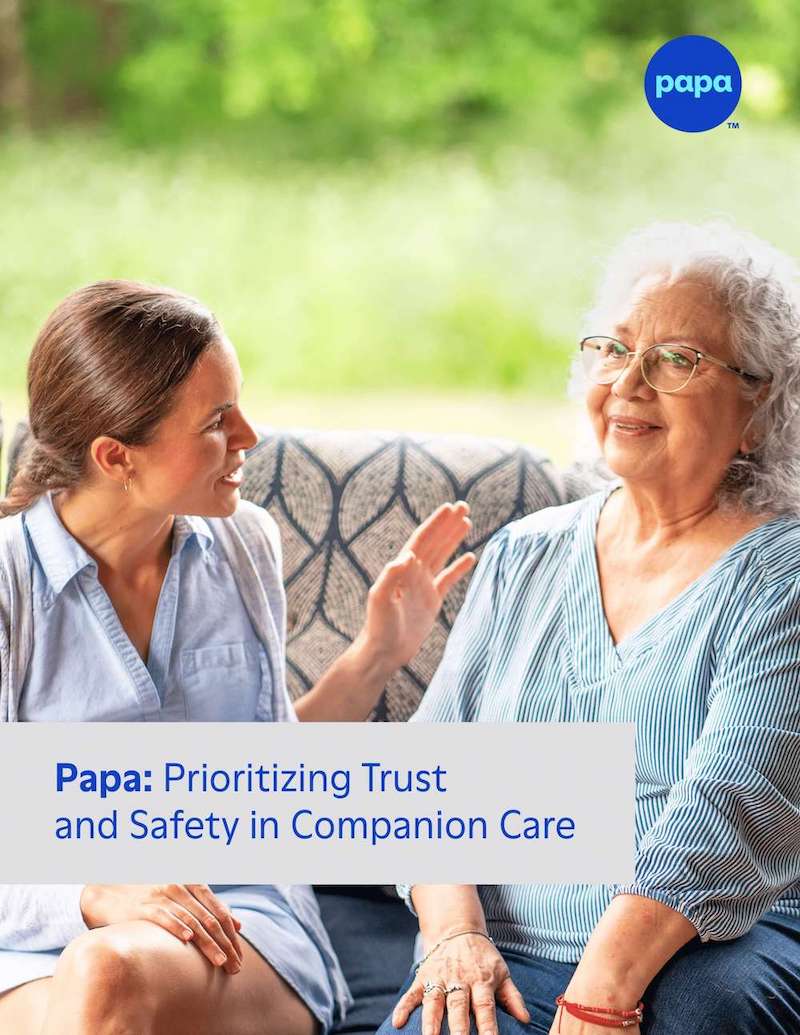
Discover how Papa has raised the bar for what it means to be a safe and trusted companion care platform.
Papa’s inaugural transparency report
Interested in Papa for your members?
Do you work for a health plan and are interested in offering our companion care services to your members? Want to learn more about how Papa can benefit your health plan members? Let’s chat!
Fill out the form below to receive a response from our team or contact us directly at sales@papa.com.
Are you a care provider, social worker, or health plan representative interested in connecting an individual with Papa’s services? At this time we only offer companionship services to eligible health plan members. Please reach out to their health plan or insurance to see if they offer Papa services and for more information.
*Papa presently does not provide services directly to individual consumers. Please be aware that responses to this form submission are intended solely for inquiries from health plan or employer organizations. Any other inquiries will not receive a response.