Papa is a first-of-its-kind solution using technology to deploy personalized, community-level care to older adults, underserved populations, and families at scale. Learn more about our offerings below.
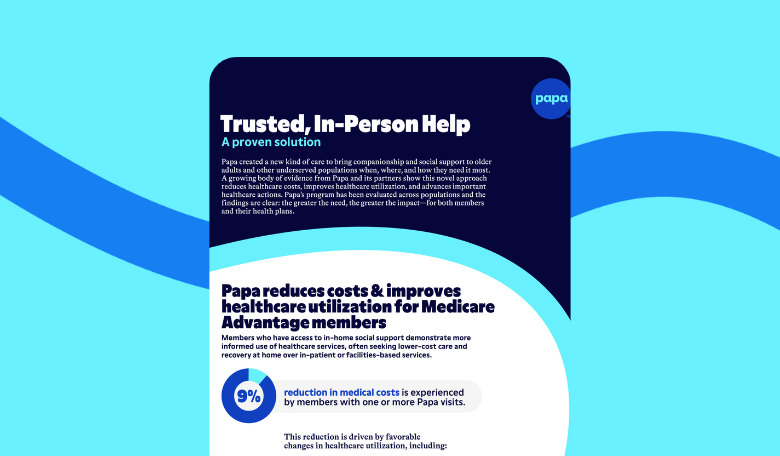
A New Kind of Care

The Papa platform
We do what technology alone cannot—provide real human connection and support to address the social drivers of health that impact upwards of 80% of health outcomes and provide much-needed respite for family caregivers. Here’s how we do it.
Papa Pals
World-class operations
Best-in-class technology platform
Expert social care navigators
Solutions & Offerings

Core Companionship
A national network of empathetic Papa Pals provide in-person and telephonic companionship and assistance with everyday tasks. Papa Pals give your members or employees the vital social support they want and need, from rides to the grocery store to respite from caregiving responsibilities to social interaction and much more. Review our health plan and employer pages for more information on how Papa can benefit your population.

Targeted Enrollment
Rather than a one-size-fits-all, Papa can tailor enrollment to reach the members or employees who need us most—generating the greatest impact and highest savings. Our team can make data-backed recommendations on populations to target and/or take your lead on where you’d like to focus resources.

Digital Health Literacy
Papa’s Digital Health Literacy program, which can be layered on top of core companionship, bridges the care access gap and addresses a new CMS health equity requirement for Medicare Advantage plans to identify and offer digital health education to their members. Learn about Digital Health Literacy.

Post-Discharge Support
Health plans can add post-discharge support to core companionship or leverage as a standalone program to ensure members transitioning home from a hospitalization receive an extra layer of care. Papa Pals fill gaps in social support to enable recovery at home, encourage discharge plan adherence, and optimize utilization of plan benefits to ultimately reduce avoidable readmissions. Learn more.

In-Home Assessments
Health plan clients can further leverage our national network of Papa Pals to complete assessments while in the home with members, including safety and health risk assessments. With a consistent presence in the home and established member relationships, our Papa Pals are uniquely positioned to gain critical member insights and report them back via the Papa Pal app. Contact us to learn how you can add in-home assessments to your core companion care program now.