You might not expect something as simple as a friend to yield a 20% reduction in emergency department (ED) visits, an 11% reduction in hospital readmissions, or a 19% increase in primary care visits. But people need people, especially when it comes to their health.
At Papa, we’ve always understood this and have focused and invested in research and impact to prove it. Six-plus years since our founding, we have a growing body of evidence—both in numbers and in smiles—that shows companion care’s clear value.
As healthcare costs rise, value reigns king
As Medicare Advantage (MA) organizations face rising healthcare costs, slimmer margins, and mounting regulatory pressures, they need to be able to show real, tangible value for every dollar spent. This means now more than ever, supplemental benefits must be able to clearly articulate impact for both members and their health plan partners.
This is a concept we understand well at Papa. Creating and scaling a category-defining model requires continual monitoring, measuring, and adapting based on results. We use evidence to inform our service development and delivery, which are ever-evolving. Let's unpack some of that evidence together.
Reducing healthcare costs and improving outcomes
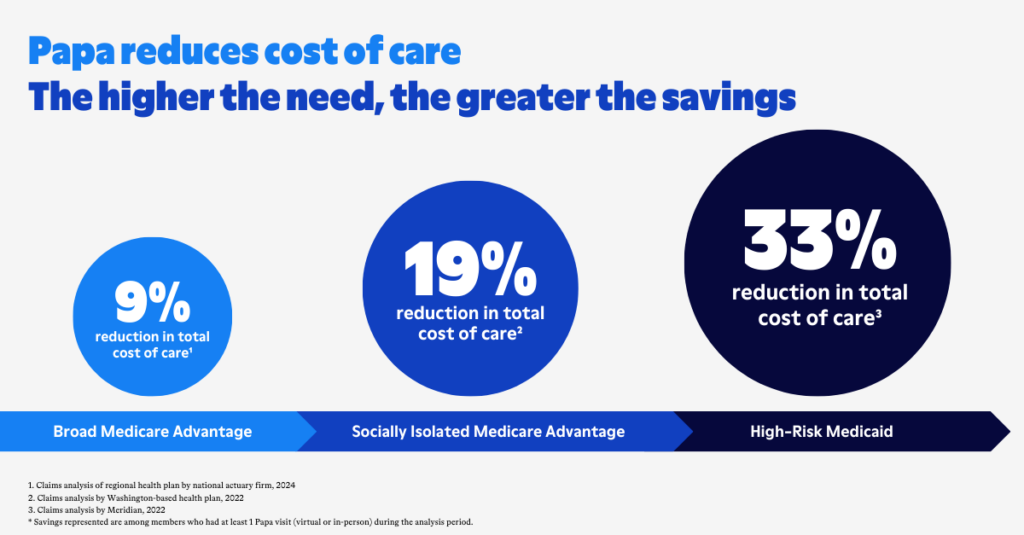
What we've found is that Papa reduces healthcare costs, and this is true across populations. The higher the need, the greater the impact, as you can see here:
- Broad Medicare Advantage population – A 2024 analysis by a leading actuarial firm of claims data for 2,300+ Medicare Advantage members found that one or more Papa visits were associated with a 9% reduction in medical costs. And completing more Papa visits was associated with even greater cost reductions—showing the potentially exponential impact long-term connection can have on an individual’s health. This includes a:
- 19% reduction in medical costs for members who average more than two Papa visits per month
- 30% reduction for members who average more than three Papa visits per month
- Socially isolated Medicare Advantage population – A 2022 claims analysis by a Washington-based health plan among 2,000+ MA members who were identified as socially isolated found a 19% decrease in medical costs among members who took at least one Papa visit.
- High-risk Medicaid population – A separate 2022 analysis by a Michigan-based health plan of Medicaid members aged 45+ with a high rate of ED utilization found a 33% reduction in healthcare costs for active Papa participants.
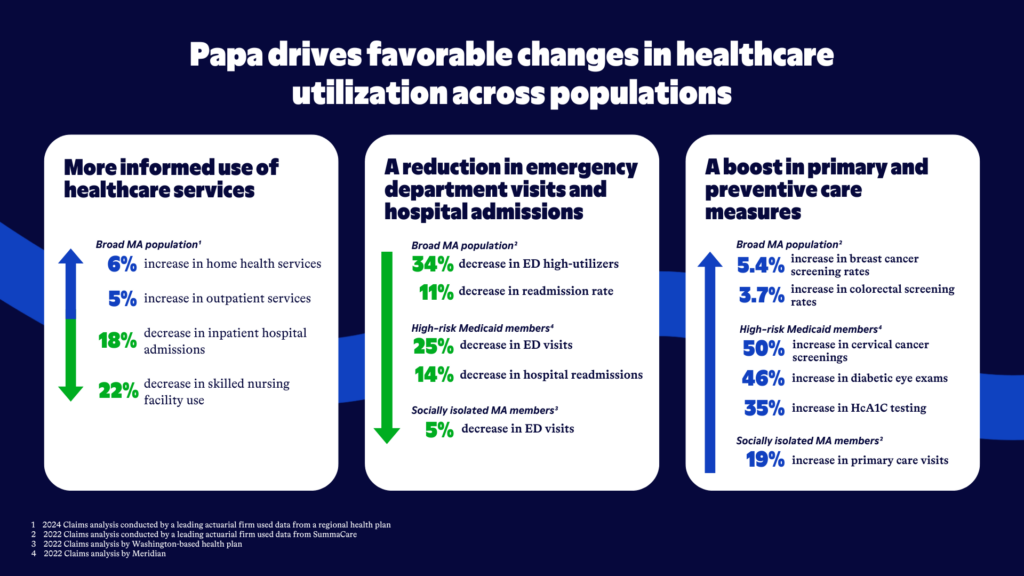
These dramatic cost savings are driven by favorable changes in healthcare utilization, including:
- More informed use of healthcare services, with Papa members often seeking lower-cost care and recovery at home over in-patient or facilities-based services. We saw this in the 2024 claims study referenced above, as MA members who took at least one Papa visit experienced an:
- 18% reduction in inpatient hospital admissions
- 22% reduction in skilled nursing facility use
- 6% increase in home health services
- 5% increase in outpatient services
- A reduction in both emergency department visits and hospital admissions across populations, including:
- 34% fewer ED high-utilizers (members with four or more ED visits during the intervention year) among Papa members, compared to a matched cohort of non-Papa members, and an 11% decline in readmission rate after enrolling in Papa, according to a 2022 analysis of 1,420 SummaCare Medicare Advantage members, conducted by an actuarial firm
- A 5% decrease in ED visits for socially isolated MA members
- A 25% decrease in ED visits and a 14% decrease in hospital readmissions for high-risk Medicaid members
- A boost in primary and preventive care measures, which allow for earlier and more accurate diagnoses and a reduction in emergency department visits—the most costly site for routine care—including a:
- 19% increase in primary care visits among socially isolated MA members
- 5.4% increase in breast cancer screening rate and 3.7% increase in colorectal screening rate among broad MA members when compared to a matched cohort of non-Papa members, according to the 2022 SummaCare claims study
- 50% increase in cervical cancer screenings, 46% increase in diabetic eye exams, and 35% increase in HcA1C testing among high-risk Medicaid members after Papa participation
These findings contributed to the reductions in medical costs outlined above, and they’re in addition to revenue plans experience from improved member experience and reduced member churn.
In fact, one study of a Florida-based health plan, conducted by health economics research firm DataMed Solutions, found Papa participants had a churn rate that was 15.8% lower than members who did not participate in Papa. Assuming a health plan has a member population of 100,000 enrolled lives and a revenue per enrollee of $12,828 (the annual healthcare costs per average Medicare enrollee in 2022 when this study was conducted), the Papa program potentially results in an incremental revenue of approximately $2.9 million.
Building evidence-based impact programs
Together, these findings validate our novel approach to meeting the health-related social needs that disproportionately drive health outcomes. They also serve as the basis for ROI estimates for our health plan partners, seeing that medical cost savings alone cover the cost of the Papa program.
This growing body of evidence also informs the evolution of our service. With this data, we have a clear understanding of where our program has measurable impact. And from years of closely partnering with our health plan clients and aligning with evolving priorities from CMS, we know what matters most to government-sponsored health plans.
And so at the areas of intersection, we develop impact programs that advance our health plan partners' most important objectives, like enhancing CMS Star Rating measures, improving successful connections to community resources for health-related social needs, and meeting new CMS health equity requirements.
These new impact programs—Star Enhancement, SDoH Navigation, and Digital Health Literacy, to start—are backed by data. More data, that is. Some of it comes from observing where our Papa Pals are naturally effective, like in uncovering members’ unmet needs and supporting members’ technology needs. It also comes from pilot programs we’ve developed with clients over the years, including programs to increase flu vaccinations and home health visits, and another to close Stars-related chronic condition care gaps among rural members, which resulted in a 6% higher composite care gap compliance rate for Papa members when compared to the matched non-Papa group.
We’re only just beginning
At Papa, we’re laser-focused on delivering positive outcomes for our members and health plan clients, while contributing to lower healthcare costs. This means continuing to measure, innovate, and partner closely with plans to test where else our unique model can make a major impact.
We believe the applications are nearly endless.
And as we roll out more and more impact programs to allow plans to be targeted and measured with how they apply our model (and how they spend their increasingly precious dollars), we’ll continue pushing the industry towards more proactive, human-centered care. Because if there’s one thing we can take away from this mountain of proof we’ve accumulated, it’s that companion care has the power to solve health care’s biggest challenges.
More about research rigor and innovation at Papa
Since the beginning, we’ve committed ourselves to building on existing evidence around the benefits of addressing social drivers of health, including the impact on health and costs. We do this in a few ways.
First, we use evidence-based, validated, and standardized tools to measure our impact, such as the widely used UCLA Three-Item Loneliness Scale, CDC Healthy Days Measure, and other social needs assessments. Using validated tools ensures we are effectively measuring the questions we seek to answer and that the tool is suitable for the population in which it’s being used, while increasing confidence in outcomes and allowing for comparison across interventions.
Second, while there are challenges evaluating real-world data and implementations, we aim for as much rigor in our research as possible. Retroactively matching cohorts can be a challenge, for example, as members who need more support are more likely to seek out Papa and are thus inherently different from their peers. Additionally, as a filed benefit, we cannot withhold our services from half the population making it challenging to conduct randomized controlled trials. With these limitations, we look for opportunities to conduct more rigorous studies in smaller settings or different types of implementations.
Additionally, to minimize biases in our studies and outcomes, our internal Research and Impact team partners often and closely with third-party actuarial firms and academic institutions. We also sometimes rely on health plan partners, who may choose to conduct their own studies and claims analyses to measure Papa’s impact and effectiveness.